Changing Demographics: Older Adults in Group Quarters

The demographic landscape of Virginia has seen significant changes over the past century, particularly the increase in the older population. While many older adults prefer to stay in their homes and communities, some inevitably transition to long-term care facilities, such as nursing homes, skilled nursing facilities, and in-patient hospices. This transition occurs when their home environments can no longer support their complex medical conditions, when they lack access to nearby community and healthcare infrastructure, or when they have limited social support from families and friends. Understanding the living arrangements of these older adults in long-term care settings is essential for informing policymakers to help guide the allocation of funds, which eventually can support direct care workers in providing services to older adults. In this blog post, we explore the changing living arrangements of older adults in Virginia, with a particular focus on those in group quarters (GQs). This exploration sheds light on the evolving needs and choices of older Virginians.
Defining Group Quarters (GQs)
Before we dive into the data, let’s clarify what we mean by “group quarters.” GQs are facilities owned or managed by organizations that provide housing and services to their residents. Typically for older adults, these facilities encompass a range of settings, from nursing homes and skilled nursing facilities to in-patient hospices, residential treatment centers, and group homes for adults. In essence, GQs offer a collective living environment, especially for older adults who require varying levels of care and support. GQs are distinct from “household” living arrangements, defined as living in their own homes, a senior housing apartment, an assisted living facility, or an independent living community.
Growth of Older Population in Virginia
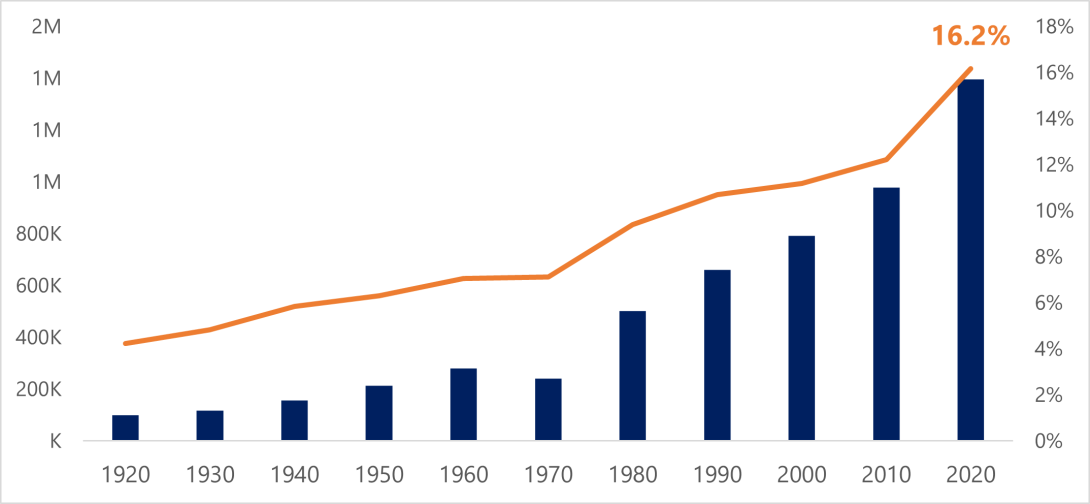
Over the past century, Virginia’s population aged 65 years and above has shown a consistent upward trajectory. This trend is evident in Figure 1, which illustrates the number and percentage of 65+ older adults in Virginia, as recorded in the decennial censuses since 1920. The data tells a compelling story of growth – in 2020, the older population in Virginia exceeded 1.3 million individuals, accounting for 16.2% of the state’s total population. This marks a significant growth from 1920, when the older population stood at around 97,000 individuals, making up only 4.2% of the total population at that time. The demographic surge in the older population is further underscored when examining the decade from 2010 to 2020, showing a 42.8% increase in the 65+ older population, compared to a 7.9% change in Virginia’s total population.
Changes in Older Adults in Group Quarters
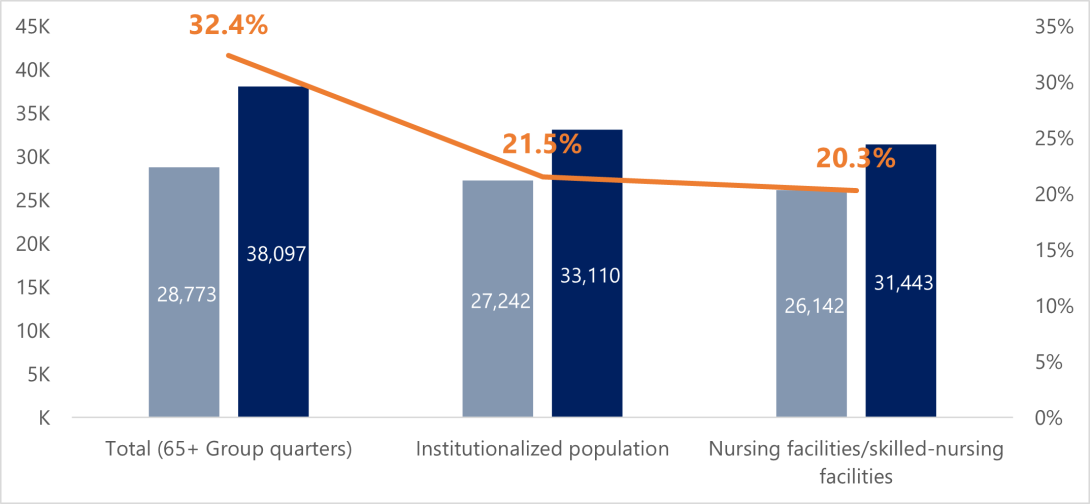
Figure 2 illustrates the change in the GQ population from 2010 to 2020, which saw a 32.4% growth. GQ residents aged 65 and above represented roughly 3% of the total older population in both 2010 and 2020. This means that while the “pie” of the older population residing in GQs has grown, the relative volume of GQ residents remained relatively stable.
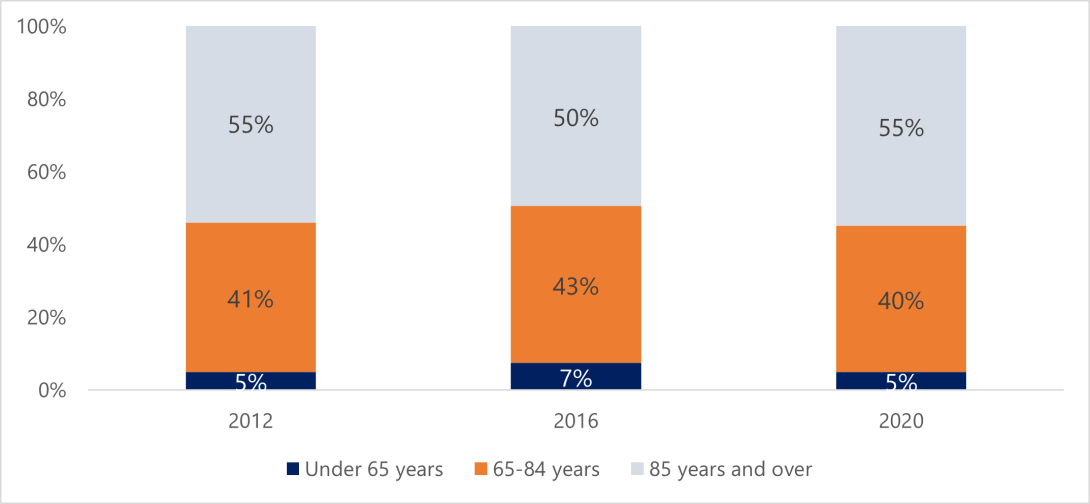
Among the 65 and above age group in the GQ population, there has been a 21.5% growth in the institutionalized population, primarily driven by a 20.3% increase in older adults living in nursing and skilled nursing facilities, though this growth rate is slightly lower than the overall growth in the older population. Notably, the number of older adults in non-institutional facilities has more than tripled, rising from 1,531 in 2010 to 4,987 in 2020, although they consisted of only 0.2% of the total 65+ population in 2010 and 0.4% in 2020. This expansion is largely due to the rise in the category of “other non-institutional GQ facilities”, such as group homes and residential treatment centers. The substantial growth of older adults living in non-institutional facilities suggests a broader trend of individuals seeking diverse living arrangements while receiving specific levels of care, all while remaining integrated within their communities rather than being institutionalized. It’s noteworthy to mention that data from the CDC’s National Center for Health Statistics reveals a consistent age distribution of residents within residential care communities over the past decade (see Figure 3), implying that this shift is not due to an increase in a specific age group within the population.
Additional Notes
The COVID-19 pandemic significantly impacted data collection for the 2020 Census, including group quarter population, leading to changes in enumeration methods, use of count imputation, and likely undercounting. Factors, such as deaths due to COVID-19 in nursing homes and residents leaving GQ facilities to live with family members during the peak of the pandemic in 2020 may have resulted in underreporting and undercounting of this population.
Nonetheless, this blog post serves as a starting point, encouraging us to consider the diversifying needs for group quarter living arrangements and care for older adults in Virginia. By understanding the shifts in living arrangements, we can better address the needs and preferences of our older population. This knowledge is not only relevant to researchers but also to policymakers, service providers, and older adults themselves as they navigate the journey of aging in our society.


